In continuation with the efforts described in the "Project Restoration" posts (#1 and #2), I'm supposed to do a therapy thing at the end of each week, sometimes reluctantly, involving "visual-neural impulse/response remapping".. brain stuff, not to be taken lightly.
This process combines a form of silent meditation with neuropharmacology — reprocessing memories via old photos while blasting the prefrontal cortex with supra-physiological dopamine levels. The Blood-Brain-Barrier must be crossed, and it must be strictly timed and controlled, while ensuring sufficient "ripcord medication" is available to halt the process.
This is achieved via prescribed medication, nothing particularly fun unfortunately, applying a timed combination of precursor + releasing agent + receptor agonist + potentiators CYP450-3A4 and CYP450-2D6. Regardless of the prescribing aspect, the combination is finely tailored to my neuro-chemistry and has been adjusted over the course of years - it is not for broad consideration or recommendation. In varying ways over the past three years, these dopaminergic alterations have been extremely challenging to manage, process, adapt, adjust, and come to terms with in their entirety.
Neural reprogramming via dopamine therapy is exceedingly dangerous territory when not managed correctly, and is not to be considered any kind of fun or pleasurable. The risk-profile is extensive: deconstruction of self-identity, parasympathetic + autonomic nervous system malfunctions, chronic sleep deprivation, tremors, hallucinations, time-slippage, and the stripping away of sanity. The potential benefits are life changing, bordering on a form of salvation from neurological trauma and post-traumatic stress disorder.
During this time the purpose is to reprogram the brain's altered response-pathways, repairing damage from trauma and its hold on sensory processing and associative recall. Secondary improvements exist, which include taking an α1-adrenergic blocker after treatment (in this case a "non-selective inverse agonist", named Prazosin), which settles down the autonomic system.
The Evolving Science of Memory Extinction
Prior to completing my seemingly never-ending research paper, here's a synopsis on the technical aspects regarding "why this works" as a treatment for scenarios involving a Post-Traumatized Brain. That term is not as common as it should be; there are a lot of people who have experienced various forms of TBI - from mild to severe. The affliction is an often desperate condition which benefits from Polytrauma Systems of Care.
Let me count the ways in which Traumatic Brain Injury is both caused by or by which manifests its existence to the external world of the unawares.
- blunt-force impact trauma (me)
- forms of cerebral ischemia (me)
- environmental exposure leading to neurogenetic disorders
- neurodegenerative diseases like Parkinsons and Alzheimers
- severe emotional trauma causing irreparable alteration to neurotransmitter homeostasis (me)
- cerebral aneurysm, stroke, grand-mal seizures, cerebral edema, cerebral anoxia
How about some raw data analysis? Everyone loves the facts, hopefully?
The following screenshot is from a wonderful study about Sequential fear generalization and network connectivity in trauma exposed humans with and without psychopathology, which was discussed in a recent post from the Institute for Neuroscience at the University of Rochester.
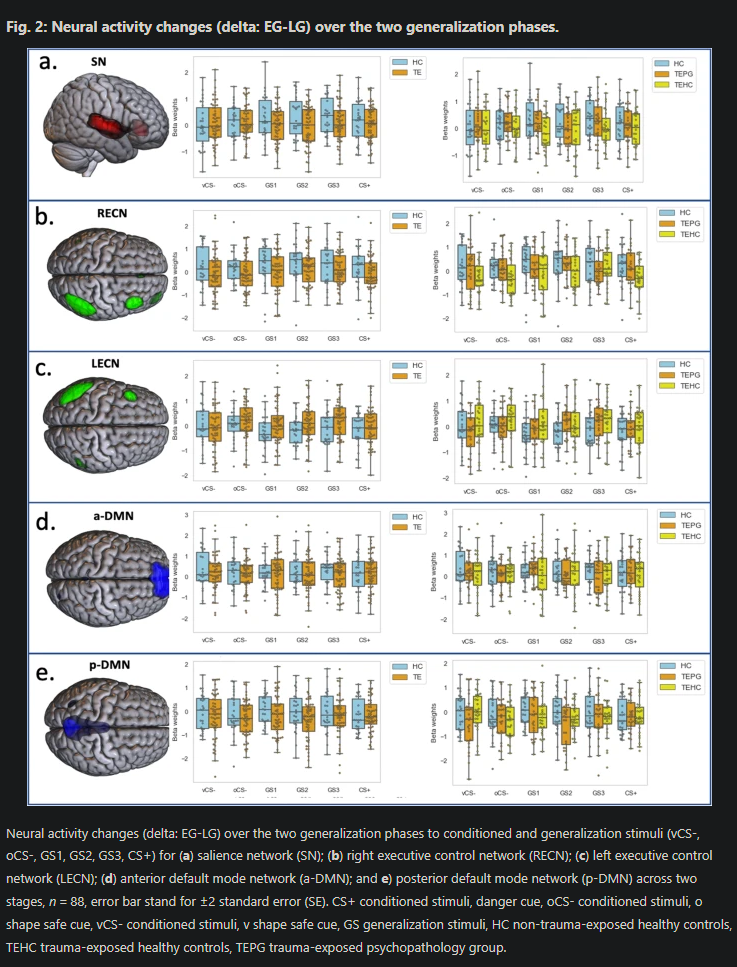
The full paper is fascinating, highly recommended reading. Moving on...
Dopamine Modulates Episodic-Memory Mapping
Why do we care so much about dopamine's role in the brain? First, consider the neurological potential which arises as a result of boosting its metabolic precursor l-3,4-dihydroxyphenylalanine, aka L-DOPA. This is an amino acid derived from L-phenylalanine and L-tyrosine, which are effectively at the top of the brain's food-chain, and when that is increased the brain has more fuel to synthesize dopamine for the therapeutic process. From the research links referenced below we have a list of essential findings and results.
Administration of L-DOPA - Key Findings
- L-DOPA after extinction consolidates context-independent extinction memory and reduces fear relapse in healthy participants.
- In women with assault-related PTSD, post-extinction L-DOPA reduced fear responding
- Mis-timed dopaminergic enhancement can strengthen reconsolidation of the original memory; careful windowing is required.
- PTSD shows broad impairments in learning and extinction; dopaminergic augmentation is a plausible lever but not standard of care.
Post-Administration Evaluation of Care and Metrics
Indeed. It's important to keep track of the results and involved metrics for the medications, doses, timing, and end-stage emotional + physical impact assessment. Considerations are given to the following list as well.
- Dose and windowing are critical to success and repeatability
- Target the post-extinction consolidation window for Cmax/Tmax levels
- Avoid dosing on "strong reactivation without extinction" to mitigate reconsolidation
- Post-care medication tracking, timing values for adrenergic and sympathomimetic reduction curves, potential fear/threat response mitigators, CNS suppressant options
Research on PTSD Dopaminergic Therapy
Before engaging in any of this mad-scientist approach to problem solving, I read a lot of research on the topic. It's an ongoing area of scientific inquiry.
While I do love science and all of its potential, I should clarify one thing: I am so goddamn tired of dealing with PTSD on an daily basis. The years of damage from sustained episodes of trauma have broken the programming structure for endogenous dopamine management, among other concerns. Not enough dopamine, you've got some big problems, as it is responsible for keeping us alive and healthy and happy and successful.
That endogenous situation is a crucial component for this form of therapy to be effective. It's not just reprogramming memories, it's concurrently back-filling the malformed neural network etchings, those disordered flows of catecholamine firing-flags (Fight or Flight Response programming: adrenaline, norepinephrine, as well as dopamine). It is a process of setting the roads straight, detangling, erasing, replacing.
- The precursor is the fuel which provides the base metabolic requirements
- The releasing agent boosts conversion of the precursor into the hormone
- The agonist tells the hormone's receptors to hang on tight and for longer
At coordinated-curves, the result is substantially higher circulating dopamine in the brain — namely the PFC (prefrontal cortex) where memory consolidation and processing occurs. Peak reprogramming requires substantially higher circulating dopamine — plus an awareness for proper management of the effects and inevitable side effects. Caution must be exercised.
This is the kind of situation where the patient has a debilitating injury for over two decades — has tried effectively everything — and are now fully into the realm of experimental approaches to "just get it fixed, somehow, please".
🧠 PTSD & Intrusive Memory Studies
Tap to expand. Search below.
1. Neuromodulation of Visual Cortex ▼
Hypothesis: Inhibiting early visual cortex during reconsolidation will blunt the affective “gain” on intrusive images.
Cause: Brief memory reactivation → 1 Hz rTMS over early visual cortex (human analogue-trauma paradigm).
Effect: Reduce visual-cortical contribution to intrusive image salience.
Observation: Emotional intensity of intrusions ↓; frequency & explicit memory unchanged.
rTMS Visual Cortex Reconsolidation
2. Traumatic Stress Alters Visual Reactivity ▼
Hypothesis: Acute trauma perturbs basic visual-cortex impulse responses that track intrusion symptoms.
Cause: Recent trauma exposure; checkerboard visual stimulation during fMRI.
Effect: Visual sensory reactivity/connectivity shifts underpin later intrusive symptoms.
Observation: Visual-cortex reactivity associates with PTSD (especially intrusion) symptoms; altered visuo-sensorimotor connectivity.
fMRI Visual Reactivity
3. Intrusive Memories: fMRI Study ▼
Hypothesis: Encoding in amygdala & ventral occipital cortex predicts which moments become intrusive.
Cause: Trauma-film encoding during fMRI.
Effect: Stronger amygdala–visual encoding → more intrusions.
Observation: Higher amygdala & ventral occipital activity at encoding predicted later intrusive memories.
fMRI Amygdala Encoding
4. Neural Basis of Involuntary Recall ▼
Hypothesis: Specific encoding patterns in visual–limbic circuits determine involuntary trauma imagery.
Cause: Trauma-film task with later intrusion tracking.
Effect: Identify visual–limbic signatures that drive involuntary recall.
Observation: Encoding activity patterns in occipito-limbic circuits predicted later intrusions/recall.
fMRI Encoding Limbic
5. Propranolol & PTSD Symptoms (RCT) ▼
Hypothesis: β-adrenergic blockade during reactivation disrupts reconsolidation, weakening trauma memory affect.
Cause: Oral propranolol before weekly trauma-memory reactivation sessions.
Effect: Noradrenergic dampening of restabilization → symptom reduction.
Observation: Greater PTSD symptom reductions vs placebo; supports reconsolidation-blockade approach.
Propranolol Reconsolidation
6. Propranolol in Chronic PTSD (DB-RCT) ▼
Hypothesis: Same as above; test efficacy in chronic PTSD.
Cause: Reactivation + propranolol vs placebo (6 sessions).
Effect: Attenuate emotional weight of memory.
Observation: Both improved; no overall drug–placebo difference; signal in most-severe subgroup.
Propranolol Chronic PTSD
7. NEJM Prazosin Trial in Veterans ▼
Hypothesis: α1-blockade during sleep reduces adrenergic drive → fewer nightmares & symptoms.
Cause: Nightly prazosin vs placebo (26 weeks).
Effect: Lower central NE tone during REM/sleep.
Observation: No benefit vs placebo on nightmares, sleep, or global PTSD.
Prazosin Veterans
8. Single IV Ketamine (JAMA Psychiatry) ▼
Hypothesis: NMDA antagonism acutely boosts plasticity to downshift pathological memory traces.
Cause: Single sub-anesthetic ketamine infusion vs midazolam.
Effect: Rapid plasticity → fast symptom relief.
Observation: Rapid PTSD symptom reduction (24h–1wk) vs control.
Ketamine NMDA
9. Repeated Ketamine Infusions (AJP) ▼
Hypothesis: Repeated NMDA modulation yields more durable remapping of threat circuits.
Cause: 6 ketamine infusions (2 wks) vs midazolam.
Effect: Strengthen extinction/modify memory networks.
Observation: Significant PTSD severity reduction; first RCT showing efficacy in chronic PTSD.
Ketamine Repeated Chronic PTSD
10. l-DOPA After Extinction (Women with PTSD) ▼
Hypothesis: Dopamine boost post-extinction strengthens safety memory to prevent return of fear.
Cause: l-DOPA/carbidopa immediately after extinction (fMRI).
Effect: Enhance consolidation of extinction (“remap” threat→safety).
Observation: Reduced reinstatement/return of fear; amygdala patterns support extinction memory.
l-DOPA Dopamine Extinction
11. MDMA Therapy & Brain Activity (fMRI) ▼
Hypothesis: MDMA-AT retunes brain networks during trauma recall, lowering visual-imagery contrast.
Cause: Active MDMA sessions within a Phase-2 protocol (pre/post fMRI).
Effect: Increase adaptive FC; dampen amygdala–insula coupling; modulate visual areas.
Observation: ↓ amygdala–insula FC; reduced cuneus contrast; trend ↑ amygdala–hippocampus RSFC.
MDMA fMRI Therapy
12. Phase-3 MDMA-AT RCTs (Nature Medicine) ▼
Hypothesis: MDMA fosters fear extinction & reconsolidation updating via neurochemical surge.
Cause: MDMA vs inactive placebo alongside fixed therapy protocol.
Effect: Reopen plasticity; enable trauma-memory “remapping”.
Observation: Large symptom reductions; many no longer met PTSD criteria.
MDMA Therapy Phase-3 RCT
This is an ongoing research indulgence, a topic very close to my heart. ❤️
Remembering the Past - Photographic Neuro-Therapy
How about some examples from this past week. Generally these are simple captures of points in time, however these are linked to specific time periods of my life when PTSD events occurred. When I see them there is a flood of emotion and physical response: elevated heart rate, deep intake followed by shallow rapid breathing, the echoing surge of norepinephrine from fight or flight response, and inevitable accompanying psychological aversion. These are the effects to be remapped, the process of meditation and cognition-alteration with which to be engaged.
Considerations of Creative-Emotive Outlets

I used to love painting, and perhaps if there were more space for all of my many projects then I would try to get back into the process. Creativity and artistic expression are relaxing and healing; it's true. Looking back, my last one was a 6'x4' canvas in acrylics, which I had finished for a contract-design.
After the "assault by gunpoint incident" I simply could not hold a brush, could no longer see the future of the paints upon the canvas, no longer imagine beautiful images finding their way from mind-to-hands. Creativity in that manner simply ceased, and I've not been able to resume. Having to stop was like losing part of my identity, connection to passion, vibrancy.
Coming to Terms with Physical Scars

Circa a few years after the coma, we see those two scars which never heal. Sometimes I put concealer on them, sometimes I lose interest in covering them for the sake of the visual public. I've written so much about this already, there nothing much new to say right now. I returned, and I live with that fact — feeling every moment.
Early Life and Times in a San Francisco Career

The innocent early years in SF, commonly engaged in expressions of "overly formal" attire for the west coast tech industry. Those occurred at the same time as the gun violence, domestic violence, and desperation-inducing medical trauma. So, how does one already trauma-laden young woman cope with more, while attempting to climb the corporate ladder? Any way she can, an escape artist, international travel, constantly moving, preferring to replace the pain with newness and knowledge.
Coping with a Returning To American Life

There is only so much to say about my most recent return to the USA, moving back to take a mostly-dream job running a hardware research lab. This photo was taken during the initial months when my PRL level began to skyrocket off the reference range; that growing trendline on the many successive blood tests proving tumor growth on the Anterior Pituitary Gland; the Suprasellar-Fossa Meningioma and its migraine inducing Optic Chiasm concerns would arise some years later.
The anterior pituitary secretes a number of peptide and glycoprotein hormones that regulate various cellular processes including growth, metabolism, reproduction, and response to stress or trauma. The hypothalamus regulates the anterior pituitary via secreting "releasing hormones", somatostatin and dopamine.
The physicians in America ignored my concerns, ignored the labs, ignored everything about this brain tumor for FIVE YEARS until an eventual MRI was ordered. Memories from those five years are extraordinarily difficult to remap, part of an ongoing source of simmering rage underscoring every medical encounter with that health organization. The pituitary tumor was only one marker in a complex set of endocrine system dysfunctions. Regulating its effects in the early stages would have prevented a chain of events from which my body will never return to baseline.
So much physical pain, emotional suffering, and secondary orders of impact could have been prevented if only they had listened (if only anyone had listened) to this one woman's reproductive system concerns. The medical industry doesn't care about women - we're not often profitable enough. Now eight years later, symptom remission requires a forever-expensive and stressful managed condition, but at least thus far I've avoided invasive brain surgery.
Parting Thoughts for Project Restoration
The past is not so easily escaped, nor resolved, or often acknowledged — and so it may never heal. However, with sufficient care perhaps these memories may be laid to rest, if not remapped by way of modern self-administered neuroscience miracles. ❤️